World-Record Achievement
Breaking barriers in cardiac surgery with the smallest incision ever recorded
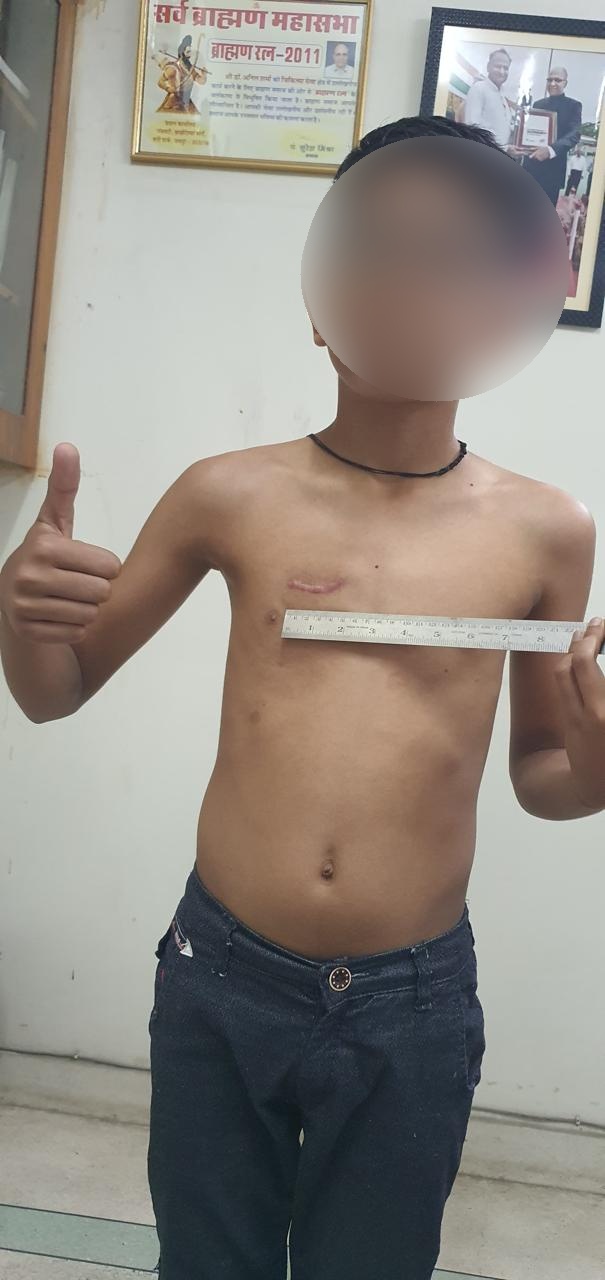
Smallest Incision in Open-Heart Surgery
On March 20, 2023, Dr. Anil Sharma achieved a world record by performing open-heart surgery through the smallest incision ever recorded. This groundbreaking technique revolutionizes patient recovery, reduces scarring, and sets new global standards in minimally invasive cardiac surgery.